Connect With Us
Blog
Blog
A Comprehensive Overview of Athlete’s Foot

Athlete's foot, a common fungal infection, unfolds as an uncomfortable and often itchy condition affecting the feet. This ailment thrives in warm and damp environments, making sweaty socks and tight shoes an ideal breeding ground for the fungus trichophyton. The infection typically begins between the toes, presenting as redness, itching, and a burning sensation. As it progresses, athlete's foot can lead to the development of blisters and the peeling of the skin. Beyond the discomfort, this contagious infection can spread to other parts of the body or to others through contact. Prevention involves keeping feet dry, wearing breathable footwear, and practicing good hygiene. If you have any of the above symptoms, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose this condition and prescribe medication, if warranted.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
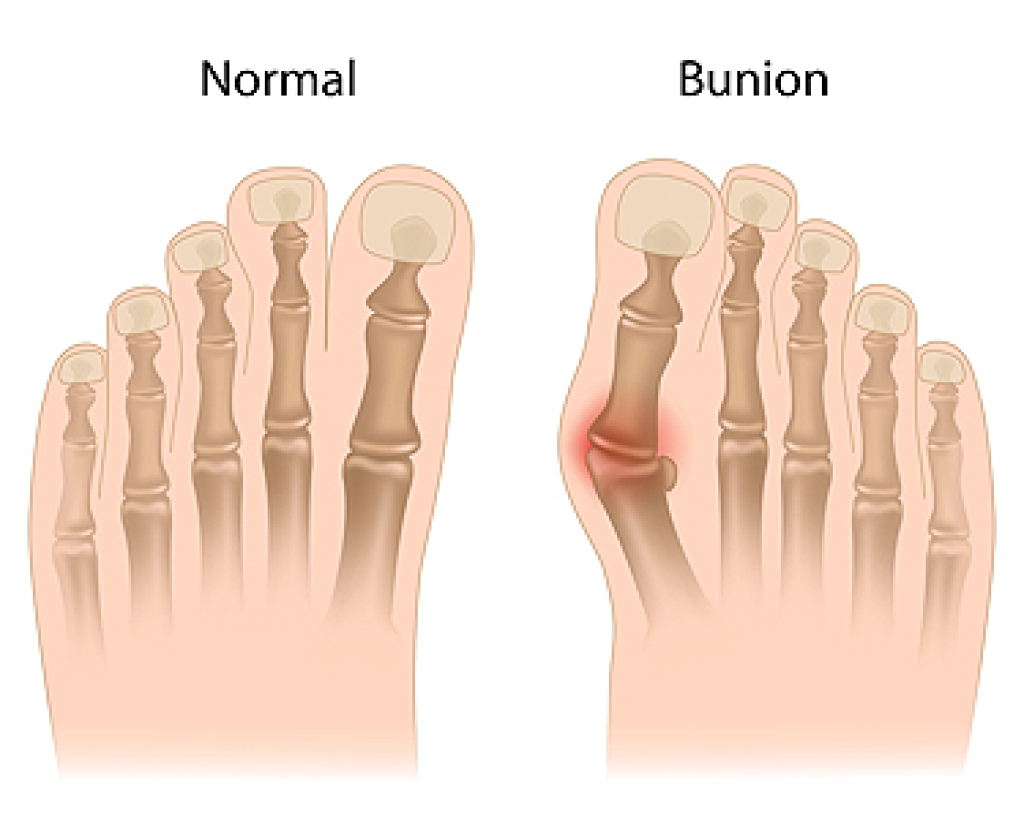
Non-Surgical Treatment of Bunions
A bunion, a bony protrusion at the base of the big toe, results from bone, tendon, and tissue misalignment. This condition causes the big toe to angle towards the smaller toes. Non-surgical treatments aim to manage pain, reduce swelling, and slow bunion progression. Appropriate footwear plays a vital role, and choosing spacious, bunion-friendly shoes that allow toe room is essential, while avoiding pointed or tight shoes is advisable. Wearing orthotics can improve comfort, arch support, and weight distribution. Additionally, splints and toe spacers can help maintain toe alignment and alleviate pressure on the toes. Engaging in specific exercises can enhance flexibility, relieve pain, and strengthen foot muscles. Although these methods can alleviate symptoms and slow bunion progression, they do not correct the underlying bone misalignment. Surgery may become necessary for severe pain or when conservative treatments prove ineffective. If you have a bunion that is causing discomfort, it is suggested that you schedule an appointment with a podiatrist for pain-relieving treatment.
If you are suffering from bunions, contact Jeffrey Radack, DPM of Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flip Flops May Cause Possible Harm to the Feet

While flip flops may be a staple of warm weather wardrobes, they pose a significant risk to the health of our feet. These flimsy sandals lack proper arch support and cushioning, exposing our feet to a host of issues. The flat, thin soles fail to absorb shock, leading to increased pressure on the heels and arches, which can contribute to conditions like plantar fasciitis. The lack of ankle support also increases the risk of sprains and strains. Additionally, constant gripping to keep flip flops in place can lead to toe deformities and exacerbate existing conditions, such as bunions. The open design exposes feet to external elements, making them susceptible to injuries, infections, and sunburn. Long-term use of flip flops can result in altered walking patterns, affecting overall posture. To safeguard foot health, it is essential to choose footwear that provides adequate support and protection, relegating flip flops to short-term, low impact use. If you are interested in additional information about the impact flip flops may have on the feet, it is suggested that you schedule an appointment with a podiatrist.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Strategies to Prevent Falls in Every Room at Home

Creating a safe environment within each room of your house is vital to preventing falls and promoting overall well-being. In the bathroom, install non-slip mats and grab bars near the shower and toilet to enhance stability. Keep pathways clear in the living room, securing loose rugs and removing clutter that might pose a tripping hazard. Adequate lighting in the bedroom is essential for visibility, reducing the risk of stumbling in the dark. In the kitchen, ensure spills are promptly cleaned, and arrange commonly used items within easy reach to avoid unnecessary stretching or bending. Staircases demand sturdy handrails and proper lighting to facilitate safe navigation. Regularly inspect and maintain flooring in all rooms, addressing any uneven surfaces promptly. By incorporating these preventive measures throughout your home, you create a secure living space that minimizes the likelihood of falls, allowing you to move confidently and enjoy every room without the worry of potential accidents. If you require additional information about implementing fall prevention techniques which may help to protect the feet, it is suggested that you speak with a podiatrist.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Assessing Diabetic Foot Ulcers

Diabetic foot ulcers are difficult wounds to heal because they can be caused by many factors. Podiatrists have different ways to treat these ulcers, including looking at blood flow problems. Neuroischemic ulcers develop from poor blood flow and nerve damage in the feet, making up approximately half of the cases of diabetic foot ulcers. When a patient has a diabetic foot ulcer, a podiatrist looks at their entire health history, asks about their daily habits, and checks how well they can move and complete everyday activities. The foot doctor also needs to know what medications the patient is taking, as some can slow down healing. All this information helps them determine the best way to treat the ulcer. The top goals are to find out what is causing the ulcer, determine how to stop it from getting worse and encourage the patient to follow the treatment plan. If you have diabetes and have developed a foot ulcer, it is strongly suggested that you make an appointment with a podiatrist as quickly as possible for a thorough assessment, examination, and treatment plan.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes and Symptoms of Foot Stress Fractures

Foot stress fractures, prevalent among runners, are primarily attributed to overuse, constituting 80 percent of cases. The repetitive forces during running may cause microscopic bone damage, escalating into hairline fractures if adequate recovery time is not provided. Sudden increases in running volume, intensity, or frequency, common in the overtraining syndrome, can make it worse. Running form also plays a role, especially with those who have a pronounced heel strike. However, transitioning abruptly to a forefoot strike or wearing minimal footwear can similarly increase the risk of metatarsal stress fractures. Nutrition is a vital factor in preventing stress fractures of the feet. Low vitamin D levels, specifically during winter, elevate the risk of stress fractures. Runners, especially women, face heightened risk if conditions such as osteoporosis or menstrual cycle-related amenorrhea are present. Additionally, sudden changes in running surfaces, such as switching from trails to roads without proper training, can elevate the risk. Wearing proper footwear is equally as important. Old, ill-fitting shoes that lack proper support can increase bone stress. Balancing training intensity, adopting gradual changes in running techniques, maintaining a nutritious diet, and ensuring proper footwear are key components of a comprehensive approach to foot health and injury prevention. For help in managing foot stress fractures, it is suggested that you schedule an appointment with a podiatrist.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Peripheral Neuropathy

Common peroneal nerve dysfunction, also known as common fibular nerve dysfunction, involves damage to the peroneal nerve, affecting movement and sensation in the foot and leg. This condition can occur at any age and is a type of peripheral neuropathy, specifically mononeuropathy, where a single nerve is damaged. Causes can range from knee trauma, fibula fracture, tight casts, habitual leg crossing, to pressure during sleep or surgery. It is also seen in individuals with anorexia, autoimmune conditions, diabetes, alcohol use, or inherited disorders like Charcot-Marie-Tooth disease. Symptoms include decreased sensation, numbness, tingling in the leg, foot dropping, a slapping gait, toe dragging, and muscle weakness. Diagnosis involves a physical exam, electromyography, nerve conduction tests, MRI, and nerve ultrasound. Potential complications may include reduced walking ability and permanent sensation loss or weakness in the legs or feet. If you have symptoms of peripheral neuropathy, it is suggested that you schedule an appointment with a podiatrist to discuss treatment options.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Can Exercises Help Heel Spurs?

Heel spurs, bony outgrowths at the bottom of the heel bone, can be a source of persistent foot discomfort. Formed due to calcium deposits, heel spurs often accompany conditions like plantar fasciitis. The pain associated with heel spurs typically arises during weight-bearing activities, especially after rest periods. While rest and proper footwear are important components of managing heel spurs, specific exercises can provide relief. Stretching exercises, such as calf stretches and towel curls, may help to alleviate tension in the Achilles tendon and plantar fascia. Rolling a frozen water bottle under the foot can reduce inflammation. Strengthening exercises, like toe-tapping and marble pickups, enhance foot and ankle muscles, promoting better support. A podiatrist treats heel spurs. If you have developed this condition, it is suggested that you visit this type of doctor who can help you with appropriate treatment and guide you toward additional stretches.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- 2025
- 2024
- 2023
- 2022
- 2021