Connect With Us
Blog
Exploring Walking and Running Shoes

Walking and running activities might seem similar to many different individuals. Both activities involve the movement of feet and motion. However, despite their similarities, walking and running are extremely different. As a result, both activities require significantly different kinds of shoes, and one shoe will not necessarily work with the other activity. There are many different reasons to help explain this. Importantly, individuals use different strike patterns when they are walking versus running. When running, the feet will strike with the heel, but not necessarily immediately roll forward onto the toes. This is not the case with walking. Additionally, running puts more force from the body's weight onto the feet when compared to walking. Consequently, both running and walking require different things in shoes tailored for that activity. If you are interested in learning more about walking and running shoes, contact a podiatrist today.
For more information about walking shoes versus running shoes, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Differences between Walking and Running Shoes
Both running and walking are great exercises, but should a person wear the same shoes for both activities? The answer is no, because there is a difference between the way a person’s feet hit the ground when they are walking and when they are running. Therefore, the shoes for each activity are designed differently. Before you begin any exercise program it is always recommended that you speak with your doctor or podiatrist.
Walking is a low impact exercise that is often recommended by doctors to their patients. While walking is a simple activity, it still requires some degree of preparation. If you think about walking and how your feet strike the ground as you move, you will notice that your heel hits the ground first before your foot continues to roll forward and your next step begins. Because of this rolling motion, walking shoes are designed to be more flexible than running shoes. This flexibility helps the walker push off with each step taken.
Because the heel hits the ground first when you walk, walking shoes are designed to absorb most of the shock. Walking shoes should therefore have a beveled or angled heel. The angle of the heel helps absorb the shock and reduces pressure from the ankles. This is especially important for speed walkers, as their feet will hit the ground twice as often as the normal walker.
When people decide to run as a hobby or for their health, they must first realize that running is a high impact exercise. If not done with the proper equipment, running may cause damage to the feet and legs. Running shoes are designed to be more lightweight and to have thicker soles. The thicker soles act as shock absorbers for the rest of the body. Walking shoes often do not have the proper arch support that running shoes do.
A proper fitting shoe can make or break a runner or a walker. If the shoes are too big, their feet will slide back and forth inside the shoe and cause blisters. Whether you will be running or walking, the right equipment can make all of the difference in the world.
Shoes and Tarsal Tunnel Syndrome

Tarsal tunnel syndrome is a lesser-known condition of the foot among the general public. This condition occurs when pressure is applied to the nerves in the ankle, sometimes causing discomfort and pain. When an individual has a case of tarsal tunnel syndrome, there are a number of steps that they might consider taking to treat the condition or mitigate the pain. One of these remedies includes wearing special shoes that are designed to combat the pain caused by tarsal tunnel syndrome. If you suffer from this foot condition, you might consider wearing shoes that relieve foot pain by essentially absorbing shock caused by weight-bearing activities. Shoes that provide extra support to the foot are also ideal for some patients with tarsal tunnel syndrome. For example, shoes that have sufficient arch and heel cushioning can provide needed support to the foot. If you have tarsal tunnel syndrome, consider contacting a podiatrist who can help you address any concerns. Schedule an appointment today.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Jeffrey Radack, DPM of Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
Most Common Foot Problems in the Elderly

Aging feet have endured years of wear and tear. It is therefore not surprising that foot problems are common among seniors. Plantar fasciitis is when the plantar fascia, the thick fibrous band of tissue that connects the heel to the toes, becomes inflamed from overuse or improper support. There can be a pain in the heel and the arch of the foot with this condition, which is more apt to be felt upon arising after rest. After walking some, the pain can subside only to resurface. Resting the affected foot, wearing orthotics, and performing stretching exercises can help this condition. Bunions form when the joint of the big toe moves out of place due to pressure. This causes a bump to develop on the side of the toe, and the toe to point inward towards the smaller toes. Swelling, redness, or soreness can develop on the joint, as well as calluses around the second toe. Bunions can cause persistent foot pain. Medications, bunion pads, splints, and wearing proper footwear that has sufficient room in the toe box can help. If you are older or take care of someone elderly who has developed a painful foot condition or wants to learn how to prevent these from happening, consult with a podiatrist who can help you.
If you need your feet checked, contact Jeffrey Radack, DPM of Texas Regional Foot & Ankle Clinics. Our doctor will attend to all of your foot and ankle needs and provide you with quality treatment.
Geriatrics and Podiatry
When people age, some common issues that may occur are bone density loss, dry skin, poor circulation, and rough brittle nails. These issues may also affect your foot health if the necessary steps are not taken to alleviate the problems.
It is important to take care of your feet because feet that are injured or diseased can affect your overall health. Having painful feet hinders your ability to do daily activities or may decrease your willingness to do the things that you need to do.
Visiting Your Geriatrician
As we age, health problems become more likely, so it is essential to visit your doctor for check-ups to ensure that you are doing the best you can to take care of your health. It is recommended to check your feet frequently for any possible cuts, bruises, swelling, corns or any other irregularities.
Taking Care of Elderly Feet
Cracked or dry feet can be treated by applying moisturizer often. It is also important not to wear old socks because the older the sock is, the higher the possibility there will be that there is bacteria there. Wear fresh socks and make sure they fit properly.
Proper foot health means that you can have a more active lifestyle and you will not be bogged down by pain. Foot health also leads to good circulation, which is paramount for overall health.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
How Peroneal Neuropathy Affects the Feet
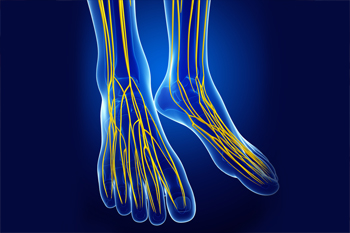
The peroneal nerve runs from the outside of the knee, down through the leg, and into the foot. It supplies movement and sensation to the lower leg, foot, and toes. When this nerve is damaged, usually by a direct trauma, it can result in numbness, tingling, or weakness in the foot. This condition is known as peroneal neuropathy. The result is a reduced ability to lift the foot to extend the toes or turn the foot outward, and may cause a kind of slapping gait while walking. This further leads to a tendency to trip, and an increased risk of a sprained ankle. It also can bring on foot drop, causing a need to lift the leg higher than normal, as in marching, to clear the floor or ground when taking a step. A loss of sensation in the sole of the foot is a common symptom. A number of imaging tests may be needed to determine the exact nature and severity of the peroneal neuropathy. Non-surgical treatment includes orthotics, braces or foot splints. In some cases surgery is required. If you are experiencing trouble lifting and moving your foot, it is a good idea to consult with a podiatrist for a full exam and diagnosis. A few neurologic conditions, such as multiple sclerosis and Parkinson’s disease, may cause similar symptoms.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is the weakness, numbness, and pain in the hands and feet due to damage to the peripheral nerves. The peripheral nerves are responsible for sending information from the brain and spinal cord to the rest of your body. Causes of Neuropathy include: traumatic injuries, infections, metabolic problems, exposure to toxins, and diabetes.
Diabetes is the most common cause, with more than half of the diabetic population developing some type of neuropathy. There are several types of neuropathy and they vary based on the damage of the nerves. Mononeuropathy is classified as only one nerve being damaged. When multiple nerves are affected, it is referred as polyneuropathy. One of the types of polyneuropathy is distal symmetric polyneuropathy. It is the most common for people with diabetes and starts when the nerves furthest away from the central nervous begin to malfunction. The symptoms begin with pain and numbness in the feet and then they travel up to the legs. A rarer form of polyneuropathy is acute symmetrical peripheral neuropathy, which is a severe type that affects nerves throughout the body and is highly associated with Guillain-Barre syndrome, an autoimmune disorder that attacks the peripheral nervous system and can be fatal. Although there are many types of neuropathy, most of them share the same symptoms such as pain, extreme sensitivity to touch, lack of coordination, muscle weakness, dizziness, and digestive problems. Since neuropathy affects the nerves, those affected should be careful of burns, infection and falling, as depleted sensations disguise such ailments.
The best way to prevent neuropathy is to manage any medical conditions such as diabetes, alcoholism, or rheumatoid arthritis. Creating and managing a healthy lifestyle can also go a long way. Having a healthy diet full of fruits, vegetables, whole grains and lean protein can keep the nerves healthy. These types of food have the nutrients to prevent neuropathy. Regularly exercising can help as well, but it is best to consult with a doctor about the right amount. In addition to diet and exercise, avoiding risk factors will also prevent neuropathy. This includes repetitive motions, cramped positions, exposure to toxic chemicals, smoking and overindulging on alcohol.
Symptoms of an Achilles Tendon Rupture

The Achilles tendon plays an integral role in the functioning of the feet. The tendon essentially connects the calf muscle to the heel bone, facilitating movement of all kinds. Since this tendon is so important, suffering an Achilles tendon injury is nothing to take lightly. An Achilles tendon rupture occurs in an individual when the tendon is stretched or torn. Typically, the tendon can stretch or tear when a person is running and they accelerate their pace too quickly. The symptoms that an individual might feel after suffering from an Achilles tendon rupture can vary. Generally speaking, however, an individual with this tendon rupture is likely to feel pain that comes in sharp, sudden bursts. This pain is typically felt in the ankle or calf. Additionally, if you are suffering from an Achilles tendon rupture, you might sense a feeling of swelling where the Achilles tendon is located, between the heel bone and the calf. Lastly, another common symptom of an Achilles tendon rupture is experiencing discomfort and difficulty when moving the feet. Specifically, walking and moving the toes can be particularly difficult. If you suspect that you have ruptured your Achilles tendon, contact your podiatrist immediately.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Jeffrey Radack, DPM of Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
What Diabetics Need to Know About Foot Care

Diabetics have high blood sugar levels that can damage blood vessels and nerves in the legs and feet. Such damage can make it hard to feel pressure, pain, and temperature in the feet. Therefore, diabetics may not know they have a cut or sore on their foot or feel the effects of shoes that are not fitting properly. Diabetes can cause the toes to become crooked or curved under and this can impact the way one walks, leading to more pressure on the foot. The increased pressure can reduce blood flow to the feet which increases the risk of foot ulcers. Diabetics need to practice regular foot care to prevent serious problems such as an infection, gangrene, or even amputation. Regular foot care involves checking the feet daily for wounds, corns, or calluses as well as changes in skin texture, color, or temperature. Wash the feet each day with warm, soapy water and dry them, followed by applying a moisturizer. Finish by trimming the toenails straight across and wear well-fitting shoes with clean, dry socks. If you are diabetic it is suggested to have a professional foot exam once a year or whenever you notice a change in your feet. A podiatrist can monitor your feet over time as well as care for any problems that may arise.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.






