Connect With Us
Blog
Diagnosis of Plantar Warts

Plantar warts, also known as verrucae plantaris, are warts that appear on the bottom of the feet, often in areas that bear weight like the heels, toes, and the middle of the foot. These warts can be particularly painful and difficult to treat because walking puts pressure on them, causing them to grow inward. Sometimes, many warts can grow together, forming what is known as mosaic warts. It can be hard to tell plantar warts apart from corns or calluses. Corns are hard skin that forms over joints from pressure and rubbing. They have a hard core and do not have the small black dots that warts do. Soft corns form in moist areas between toes due to pressure and rubbing. Another condition often mistaken for plantar warts is black heel, which can be seen in athletes like tennis or basketball players. This is where tiny blood vessels break, causing small black or brown spots on the heel or side of the foot. Carefully removing the top layer of skin can help separate this condition from warts, calluses, corns, and serious issues such as malignant melanoma. If you have what appears to be a wart on your foot, it is suggested that you make an appointment with a podiatrist for a proper diagnosis and treatment.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
Recognizing Diabetic Symptoms in the Feet

Diabetes is a condition that affects multiple aspects of your health, including your feet. Individuals living with diabetes need to be vigilant about potential foot-related symptoms, as they are at higher risk of developing complications. One common symptom is peripheral neuropathy, which can manifest as tingling, burning, or numbness in the feet. This occurs when high blood sugar damages the nerves, impairing sensation. Reduced blood flow to the feet is another issue, leading to cold or discolored skin and slower wound healing. Diabetes can also cause changes in the foot's shape, such as Charcot foot, where the arch collapses. This may lead to deformities and instability. Additionally, diabetic individuals are more prone to foot ulcers and infections. It is important to pay close attention to these symptoms, as early detection and proper management are key to preventing severe complications. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can help you to manage this condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes affects millions of people every year. Blood vessels located all over the body are damaged due to diabetes—even the blood vessels of the feet. Neuropathy, or nerve damage, can result from slower blood flow in the legs and feet. In diabetic patients, neuropathy is very important to monitor, as diabetics are at risk for developing ulcers.
Always washing and thoroughly drying the feet are pertinent parts of diabetic foot care. There should be a focus on cleaning between the toes. Even if no pain is felt, the entire foot should be examined for redness and sores. Neuropathy can often mask the pain of sores and ulcers and can cause these conditions to be overlooked. Use a mirror to examine the underside of your feet if needed. It is recommended that diabetics wear well-fitting socks.
Patients with diabetes should have their doctor monitor their blood levels because blood sugar levels play a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised. It is very important to keep your blood sugar levels in the normal range, which can be determined by your physician. There are medications that may be prescribed to help with any neuropathy experienced by the diabetic patient. It is also advisable to visit a podiatrist if one is experiencing any conditions involving the feet, such as ingrown toenails, which in more severe cases can cause infection.
Diabetic feet must be inspected daily. Diabetic foot care at home is possible if a patient is provided with instructions from their podiatrist. Patients can relieve dry heels with creams or ointments. Suspected wounds should warrant an immediate call to the podiatrist. Gangrene is a serious problem for diabetics and can lead to sepsis and amputation in its worst cases. Early treatment and daily inspection of diabetic feet are keys to staying healthy.
The Right Time to Replace Orthotics

Determining when it is time to replace your orthotics is essential for maintaining foot health and comfort. Orthotic replacement intervals vary widely, typically ranging from six months to a year, depending on individual differences in usage and wear patterns. Factors include the frequency of wear, specific footwear usage, and individual foot characteristics. Indicators that can help assess the condition of your orthotics include wear pattern and fading, lack of support and comfort, and loss of definition. Check your orthotics for worn spots or discoloration. If your orthotics no longer provide the same level of support or comfort as when new, it may be time for a replacement. Cracks, tears, splits, or deterioration in the materials signal the need for replacement. Sometimes, the need for replacement is not immediately obvious. For instance, the insert may still be in good condition, but it might have compressed and affected the built-in support of your shoes. Additionally, certain foot conditions can worsen over time, necessitating new orthotics for optimal support. If you suspect that you need new orthotics or you want to make sure you are replacing them at adequate intervals, it is suggested that you make an appointment with a podiatrist for a professional assessment.
If you are having discomfort in your feet and would like to try orthotics, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How Rheumatoid Arthritis Affects the Feet

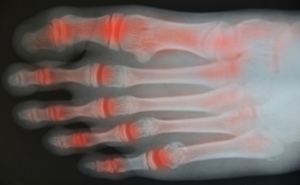
Rheumatoid arthritis, abbreviated RA, is a relentless autoimmune disorder that does not spare the feet from pain. The immune system's misguided attacks on the synovium, which is the protective lining of joints, lead to chronic inflammation in various parts of the body, including the feet. The small joints in the toes, the arch, and the ankle are frequent targets, causing swelling, stiffness, and pain. Over time, RA can lead to deformities, such as bunions, hammertoes, and collapsed arches, resulting in altered foot structure and gait. The chronic pain can impair mobility, leading to a reduced quality of life. Early diagnosis and prompt intervention are crucial to managing symptoms and slowing down the progression. A treatment approach involving medication, wearing orthotics, and incorporating lifestyle adjustments may help to alleviate the burden on the feet and enhance overall foot health for individuals with RA. If you have this condition, it is strongly suggested that you are under the care of a podiatrist who can offer you additional relief options.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Jeffrey Radack, DPM of Texas Regional Foot & Ankle Clinics. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Although rheumatoid arthritis attacks multiple bones and joints throughout the entire body, ninety percent of people who actually develop this condition usually do so in the foot or ankle area. Those who develop this kind of arthritis in the feet usually develop symptoms around the toes and forefeet first, before anywhere else. Rheumatoid arthritis appears to have a genetic component. If it runs in the family, then you will be more likely to develop it as well.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the membranes surrounding the joints. This causes inflammation of the membrane lining, and the gradual destruction of the joint’s cartilage and even bone.
Some of the most common symptoms that are associated with RA include pain and swelling of the feet. Stiffness in the feet is also another common symptom that people experience. Those who have RA in the feet usually feel the pain in the ball or sole of their feet. This can get to be very painful at times. A person's joints can even shift and become deformed after a period of time.
In order to properly diagnose RA in the feet it is usually necessary for a doctor or podiatrist to evaluate the area. Your doctor will also question you about your medical history, occupation, etc., to determine whether anything in your lifestyle may have triggered the condition. There are a number of tests that may be performed to help diagnose RA, such as a rheumatoid factor test. There is, however, no one single test that will tell you for sure if you have RA. There are different X-rays that can be taken as well to determine if a person has RA in their feet.
There is a range of treatment options for rheumatoid arthritis. Treatment of RA is usually a lifelong process that includes a variety of methods of treatment and therapy. Your doctor can prescribe special shoes that should help with arch support as well as heel support. A physical therapist can help those with this condition learn exercises which will keep their joints flexible. Surgery may be needed to correct some of the issues with the feet, such as bunions, and hammertoes. Fusion is usually the most successful surgical option for rheumatoid arthritis. However, people need to keep in mind that there are some risks associated with these surgeries.
Why Are My Feet Swollen?

People who have swollen feet are often aware of the discomfort this condition can cause. It is common among pregnant women and generally begins in the second trimester. The medical term for swollen feet is edema, which is defined as fluid that becomes trapped in the body’s tissues. The feet and ankles are common areas for this to occur, and the fluids can pool in these areas as a result of gravity. Patients who have poor circulation may experience swollen feet, or it may happen to people who have endured a foot injury. Relief may be found when the feet are frequently elevated and compression stockings are worn. It is beneficial to reduce sodium intake, in addition to drinking plenty of water daily. If you have swollen feet, it is suggested that you speak with a podiatrist who can determine the cause and offer correct treatment options.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact Jeffrey Radack, DPM of Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Swelling of the Feet
There are many reasons why patients experience swelling of the feet. It is rather common and may be a side effect of pregnancy or from sitting and standing for most of the day. Gravity could also play a role in the development of swollen feet. It is known that the weight of blood volume in our bodies is exerted on the veins in the legs and feet. The veins may not work as efficiently during the aging process, and this could make the blood flow backward causing swollen feet. Relief may be found when obese patients lose weight, and it may help to engage in compression therapy by wearing compression socks, stockings, or athletic sleeves. This method can release pressure on the feet and ankles which may help to reduce existing swelling. There are patients who have controlled their swollen feet by implementing healthy lifestyle changes. These can consist of reducing salt intake, incorporating a gentle exercise regime into the daily routine, and drinking plenty of fresh water. Swollen feet may be a temporary condition that affects people who travel via airplane or automobile, so it is beneficial to walk as frequently as possible even though it can be difficult. Swelling of the feet can also be indicative of other health issues so it is important to pay attention to any type of chest pain, mental confusion, dizziness, or fever. If you consistently have swollen feet, it is strongly suggested that you consult with a podiatrist who can help determine the cause and how to effectively treat it.
How the Foot Is Affected by Rheumatoid Arthritis
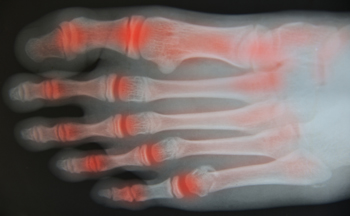
People who develop rheumatoid arthritis, or RA, are no strangers to the pain this condition can cause. The symptoms that often accompany this ailment can include stiffness, and the joints throughout the body may be swollen. The feet can be affected by rheumatoid arthritis, and it may be difficult to walk and complete daily activities. RA is considered to be an autoimmune disease, and it attacks the lining of the joints. Some patients can experience fevers, extreme fatigue, and possible weight loss. The components of the feet that are affected can include the cartilage, toe joints, and the joints that connect the foot and the ankle. Patients who are afflicted with RA look for relief, and may find it, by wearing custom-made orthotics, practicing a regular exercise routine, and maintaining a healthy weight. If you have foot pain, it is strongly suggested that you consult with a podiatrist who can diagnose and treat rheumatoid arthritis.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Jeffrey Radack, DPM of Texas Regional Foot & Ankle Clinics. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.