Connect With Us
Blog

Strategies to Prevent Falls in Every Room at Home

Creating a safe environment within each room of your house is vital to preventing falls and promoting overall well-being. In the bathroom, install non-slip mats and grab bars near the shower and toilet to enhance stability. Keep pathways clear in the living room, securing loose rugs and removing clutter that might pose a tripping hazard. Adequate lighting in the bedroom is essential for visibility, reducing the risk of stumbling in the dark. In the kitchen, ensure spills are promptly cleaned, and arrange commonly used items within easy reach to avoid unnecessary stretching or bending. Staircases demand sturdy handrails and proper lighting to facilitate safe navigation. Regularly inspect and maintain flooring in all rooms, addressing any uneven surfaces promptly. By incorporating these preventive measures throughout your home, you create a secure living space that minimizes the likelihood of falls, allowing you to move confidently and enjoy every room without the worry of potential accidents. If you require additional information about implementing fall prevention techniques which may help to protect the feet, it is suggested that you speak with a podiatrist.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Assessing Diabetic Foot Ulcers

Diabetic foot ulcers are difficult wounds to heal because they can be caused by many factors. Podiatrists have different ways to treat these ulcers, including looking at blood flow problems. Neuroischemic ulcers develop from poor blood flow and nerve damage in the feet, making up approximately half of the cases of diabetic foot ulcers. When a patient has a diabetic foot ulcer, a podiatrist looks at their entire health history, asks about their daily habits, and checks how well they can move and complete everyday activities. The foot doctor also needs to know what medications the patient is taking, as some can slow down healing. All this information helps them determine the best way to treat the ulcer. The top goals are to find out what is causing the ulcer, determine how to stop it from getting worse and encourage the patient to follow the treatment plan. If you have diabetes and have developed a foot ulcer, it is strongly suggested that you make an appointment with a podiatrist as quickly as possible for a thorough assessment, examination, and treatment plan.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Are You Suffering From Ingrown Toenails?
Causes and Symptoms of Foot Stress Fractures

Foot stress fractures, prevalent among runners, are primarily attributed to overuse, constituting 80 percent of cases. The repetitive forces during running may cause microscopic bone damage, escalating into hairline fractures if adequate recovery time is not provided. Sudden increases in running volume, intensity, or frequency, common in the overtraining syndrome, can make it worse. Running form also plays a role, especially with those who have a pronounced heel strike. However, transitioning abruptly to a forefoot strike or wearing minimal footwear can similarly increase the risk of metatarsal stress fractures. Nutrition is a vital factor in preventing stress fractures of the feet. Low vitamin D levels, specifically during winter, elevate the risk of stress fractures. Runners, especially women, face heightened risk if conditions such as osteoporosis or menstrual cycle-related amenorrhea are present. Additionally, sudden changes in running surfaces, such as switching from trails to roads without proper training, can elevate the risk. Wearing proper footwear is equally as important. Old, ill-fitting shoes that lack proper support can increase bone stress. Balancing training intensity, adopting gradual changes in running techniques, maintaining a nutritious diet, and ensuring proper footwear are key components of a comprehensive approach to foot health and injury prevention. For help in managing foot stress fractures, it is suggested that you schedule an appointment with a podiatrist.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Peripheral Neuropathy

Common peroneal nerve dysfunction, also known as common fibular nerve dysfunction, involves damage to the peroneal nerve, affecting movement and sensation in the foot and leg. This condition can occur at any age and is a type of peripheral neuropathy, specifically mononeuropathy, where a single nerve is damaged. Causes can range from knee trauma, fibula fracture, tight casts, habitual leg crossing, to pressure during sleep or surgery. It is also seen in individuals with anorexia, autoimmune conditions, diabetes, alcohol use, or inherited disorders like Charcot-Marie-Tooth disease. Symptoms include decreased sensation, numbness, tingling in the leg, foot dropping, a slapping gait, toe dragging, and muscle weakness. Diagnosis involves a physical exam, electromyography, nerve conduction tests, MRI, and nerve ultrasound. Potential complications may include reduced walking ability and permanent sensation loss or weakness in the legs or feet. If you have symptoms of peripheral neuropathy, it is suggested that you schedule an appointment with a podiatrist to discuss treatment options.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in McKinney and Coppell, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
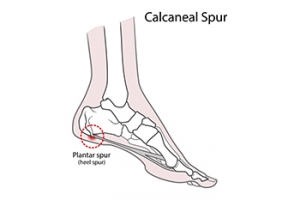
Can Exercises Help Heel Spurs?
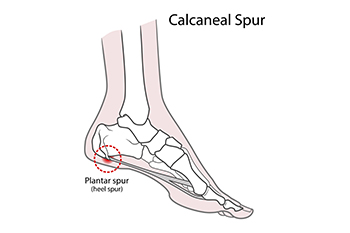
Heel spurs, bony outgrowths at the bottom of the heel bone, can be a source of persistent foot discomfort. Formed due to calcium deposits, heel spurs often accompany conditions like plantar fasciitis. The pain associated with heel spurs typically arises during weight-bearing activities, especially after rest periods. While rest and proper footwear are important components of managing heel spurs, specific exercises can provide relief. Stretching exercises, such as calf stretches and towel curls, may help to alleviate tension in the Achilles tendon and plantar fascia. Rolling a frozen water bottle under the foot can reduce inflammation. Strengthening exercises, like toe-tapping and marble pickups, enhance foot and ankle muscles, promoting better support. A podiatrist treats heel spurs. If you have developed this condition, it is suggested that you visit this type of doctor who can help you with appropriate treatment and guide you toward additional stretches.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Jeffrey Radack, DPM from Texas Regional Foot & Ankle Clinics. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in McKinney and Coppell, TX . We offer the latest in diagnostic and treatment technology to meet your needs.